Chronic Care Management
Care Prescribed by You. Managed by Us.
Our turn-key CCM/RPM solutions ensure compliance and health literacy – improving patient satisfaction and outcomes, increasing revenue, and decreasing staff workload.


Physician Assistant-owned and led—a culture of exceptional practitioner support
No upfront capital, technology costs, or resources required
Clinically-trained nurses utilize evidence-based workflows customized for physician's practice needs
Chronic Disease Burden in the United States
%
MEDICARE beneficiaries have a 2+ chronic condition
%
Patients with chronic conditions were readmitted within 30 days
%
of national healthcare costs overall
%
Americans die from chronic diseases
Examples of Care delivered by GenbyGen’s Nurses to your Patients
Medication Adherence, Refills, & Delivery Coordination

Depression and Fall Risks Screening
Scheduling Office Visits and Annual Wellness Visits

Referral Management

Patient Education and Wellness Coaching
Insurance Coordination & Benefits Optimization
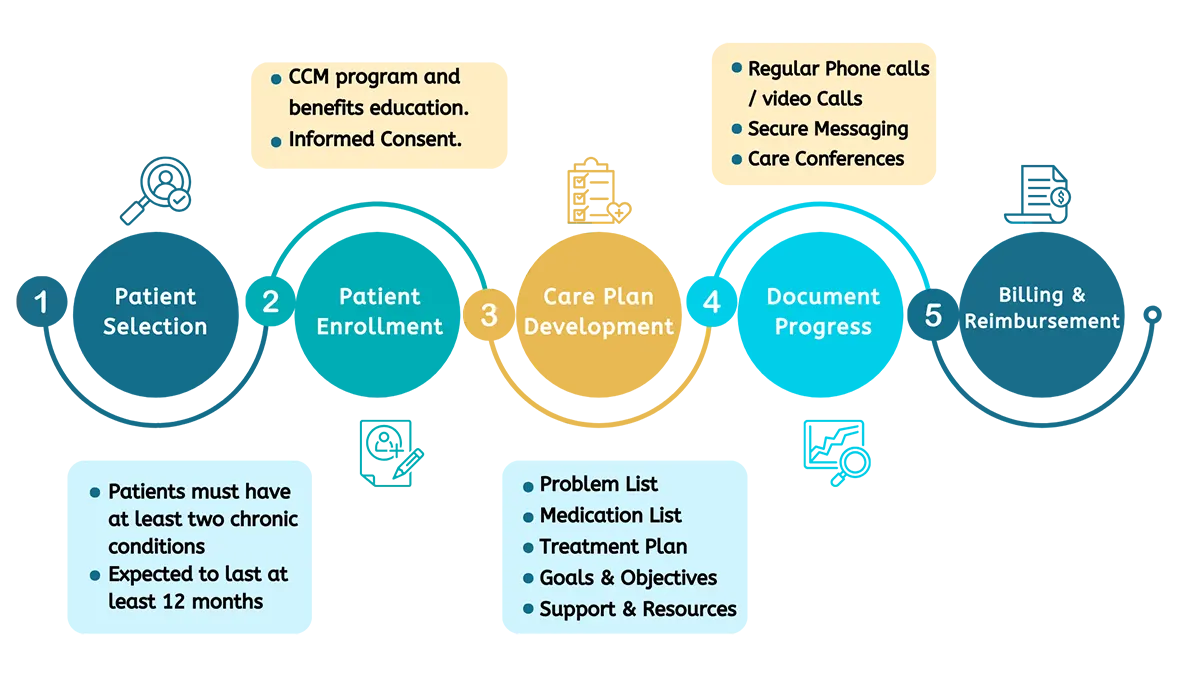
How it Works
Gen By Gen delivers successful and customizable Chronic Care Management (CCM) services by following these 5 simple steps.
A Financially Sustainable Solution
Estimate your Annual CCM/RPM Revenue
Physicians can earn $200,000+ per year through Chronic Care Management (CCM) and Remote Patient Monitoring (RPM)
Resulting in Sustainable Growth
Increase Revenue
Improve Quality Metrics
Increase Patient Engagement
Reduce Staff Workload
Our Patients’ Case Studies
Frequently Asked Questions
What is Chronic Care Management?
-
Improve health outcomes
-
increase patient satisfaction
-
Reduce healthcare costs for patients with chronic conditions
-
Care Coordination and Management: Coordinating and communicating with other healthcare providers to ensure appropriate care and tracking patient progress.
-
Care Planning: Developing a tailored care plan that is adjusted as needed.
-
Patient Education and Self-Management Support: Providing education and resources to promote self-management.
-
Medication Management: Reviewing medications and ensuring correct usage.
-
Care Transitions: Facilitating communication and coordination between patients, family members, and caregivers during healthcare setting transitions.
-
Follow-up and Monitoring: Ongoing support to maintain patient health and manage conditions over time.
Eligible Providers
CCM services can be provided by:-
Physicians
-
Nurse Practitioners
-
Physician Assistants
-
Nurses
-
Care Managers
-
Who is eligible for Chronic Care Management (CCM)?
Chronic Care Management (CCM) is a program offered by the Centers for Medicare & Medicaid Services (CMS) and is available to patients who have Medicare Part B coverage and have at least two or more chronic conditions. The chronic conditions that qualify for CCM services are those that have been or are likely to last at least 12 months and require frequent medical attention and self-management. Examples of chronic conditions that qualify for CCM services include:
CCM services include:
- Diabetes
- Heart failure
- Coronary artery disease
- Chronic obstructive pulmonary disease (COPD)
- Hypertension
- Cancer
- Depression and other mental health conditions
- Asthma
- Chronic kidney disease
- Arthritis
- Osteoporosis
- Alzheimer’s disease
- Parkinson’s disease
To be eligible for CCM services, patients must also be seen by a primary care provider or a care manager at least once every 90 days and have a care plan established with the patient or their caregiver.
It is important to note that this program is only for patients with Medicare Part B coverage.
Those who have Medicare Advantage plans (Medicare Part C) are not eligible for this program. Additionally, the patient should not be in an inpatient setting, hospice, or receiving home health services. If a patient is in an inpatient setting, then other programs such as Transitional Care Management (TCM) are more appropriate.
What are the applicable reimbursements for CCM in 2024?
| 2024 CCM Reimbursement Rates | ||
|---|---|---|
| 99490 | The first 20 minutes of clinical chronic care management services for patients with two or more chronic conditions are expected to last 12+ months. | $62* |
| 99439 | Each additional 20 minutes of clinical time directed by a healthcare professional for chronic care management services. | $47* |
| 99491 | At least 30 minutes of chronic care management services, delivered by the billing provider, for patients with two or more chronic conditions expected to last 12+ months. | $83* |
| Complex CCM | ||
| 99487 | The first 60 minutes of complex chronic care management services for patients with moderate to complex conditions. | $132* |
| 99489 | Each additional 20 minutes of complex chronic care management services for patients with moderate to complex conditions. | $71* |
What are the applicable CPT codes for CCM?
There are several Current Procedural Terminology (CPT) codes that are used to bill for chronic care management (CCM) services in the United States.
- 99490- This code is used for at least 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional, per calendar month.
- 99487 – This code is used for the initial assessment and care planning for patients with multiple (two or more) chronic conditions that are expected to last at least 12 months, or until the death of the patient.
- 99489 – This code is used for the ongoing care management of patients with multiple (two or more) chronic conditions that are expected to last at least 12 months, or until the death of the patient.
- G0506 – This code is used for remote evaluation of recorded video and/or images furnished to the patient/caregiver.
- 99458, 99459 – These codes are used for remote evaluation of patient-transmitted recorded video or image by a physician or other qualified healthcare professional via telephone, internet, or e-mail.
It is important to note that the codes and reimbursement for CCM services may vary depending on the payer, so it’s best to check with your local Medicare administrative contractor or your private payer for more information.
